Bacterial coinfection pervasiveness and antibiotic use in COVID-19 patients

In a recent study posted to the medRxiv* pre-print server, researchers conducted a meta-analysis to determine the bacterial coinfection and antibiotic usage prevalence in coronavirus disease 2019 (COVID-19) patients.
Given the similar clinical presentation of COVID-19 and pneumonia and previously reported prevalence of bacterial infections during earlier viral pandemics, bacterial coinfections due to S. pneumonia, S. aureus, H. influenza, etc., and their associated mortality and morbidity have been a grave concern during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic. This has given rise to extensive antibiotic usage in community and hospital settings. Increased antibiotic prescription against COVID-19 has increased the risk of antimicrobial resistance (AMR) and challenged antimicrobial stewardship (AMS) programs.
Although prior studies reported bacterial coinfection prevalence among COVID-19 patients, they were conducted in a small population.
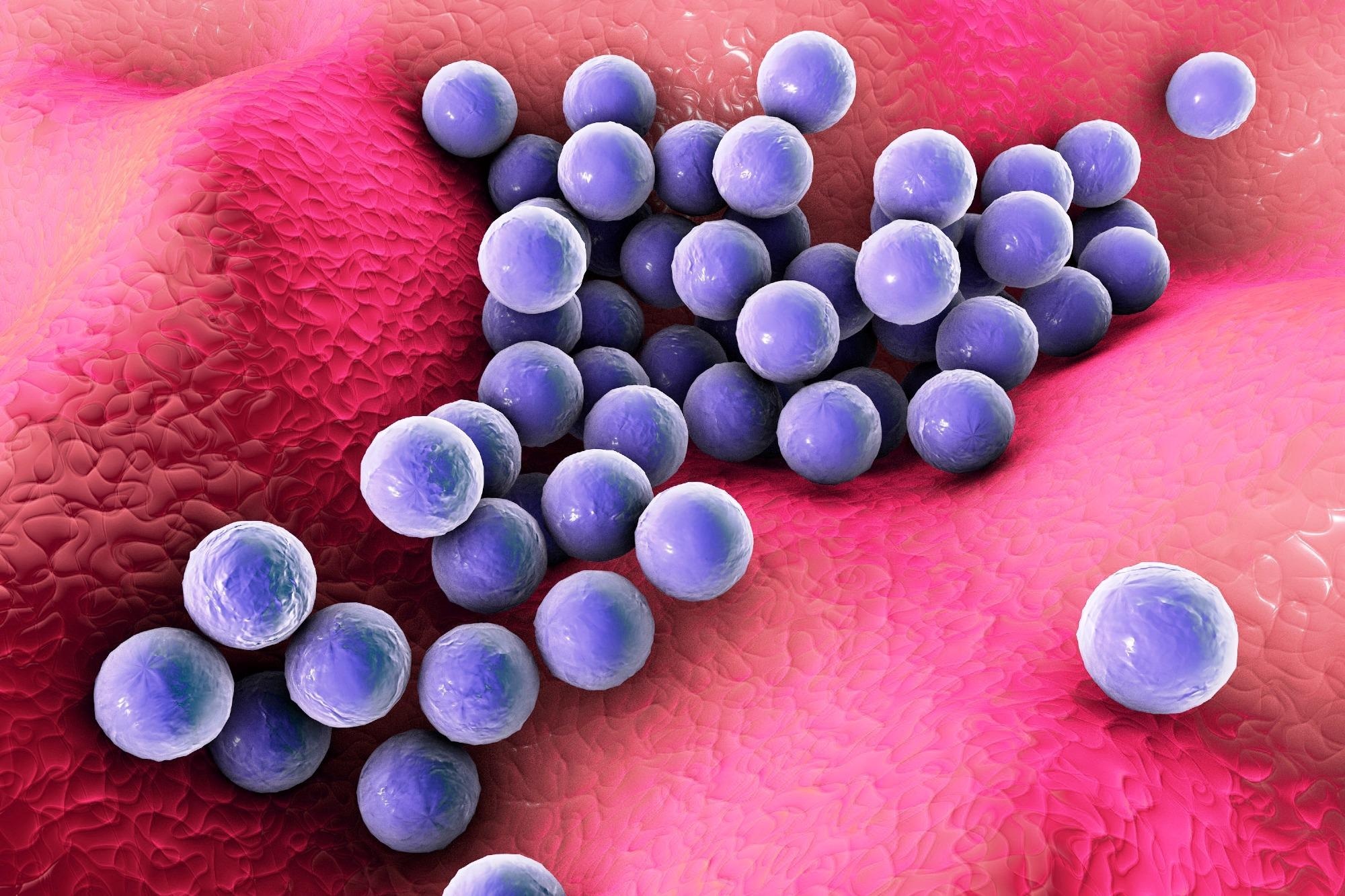 Study: Prevalence of Bacterial Coinfection and Patterns of Antibiotics Prescribing in Patients with COVID-19: A Systematic review and Meta-Analysis. Image Credit: Kateryna Kon / Shutterstock
Study: Prevalence of Bacterial Coinfection and Patterns of Antibiotics Prescribing in Patients with COVID-19: A Systematic review and Meta-Analysis. Image Credit: Kateryna Kon / Shutterstock
About the study
In the present study, the researchers conducted a meta-analysis to determine the prevalence of bacterial coinfection and antibiotic usage in COVID-19 patients.
Databases such as OVID EMBASE, OVID MEDLINE, MedRxiv, and Cochrane articles were searched for studies between December 2019 through June 29, 2021. The keywords used were “Antibiotics,” “COVID-19,” and “Coinfections.” Data were reported by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and reviewed by two reviewers, with any disputes resolved by a third reviewer.
Full text, English articles on studies performed on reverse-transcription-polymerase chain reaction (RT-PCR)-confirmed COVID-19 patients aged above 18 years that reported the prevalence of bacterial coinfection or antibiotic prescribing were included. While editorials, Case reports, letters, case notes, systematic review, and meta-analysis were excluded, pre-prints containing relevant information were included. Studies on secondary infections or/and super-infections were also excluded.
Data were obtained for variables including the publication year, first author; country of publication, study design, multicentric or unicentric hospital or communal study setting, peer-reviewed or non-reviewed; patient count, mean age, and gender distribution. In addition, data on the prevalence, most common location, causative agent, and clinical effects of bacterial coinfections; antibiotics prescribed; antibiotic initiation timing, and clinical consequences of prescribed antibiotics, if reported, were also obtained.
The primary outcomes assessed were bacterial coinfections prevalence and antibiotic usage prevalence in SARS-CoV-2 infections. A region-wise sub-group analysis was also performed, and microbiological samples diagnosed positive within two days of hospitalization were identified as a coinfection.
Results and discussion
A total of 1,183 studies were identified, from which 125 duplicates were excluded. Of the remaining 1058 studies, 22 hospital-based studies that fulfilled the eligibility criteria and comprised 56,176 patients were included in the final analysis.
The prevalence of bacterial coinfection and antibiotic usage was reported in 20/22 and 18/22 studies, respectively. Most studies (81%) employed retrospective cohort study design, the majority of studies (88%) were peer-reviewed, and more than 50% of studies were conducted in multicentre settings. Almost all (21/22) studies were classified as ‘good’ quality in the present study.
Most studies (45%) were conducted in the United States of America, followed by the United Kingdom (UK), China, France, Indonesia, Germany, Spain, and the Netherlands. The continents represented most were North America (45%), Europe (36%), and Asia (18%). From 20 studies investigating bacterial coinfections, only 4.7% of patients were diagnosed with a bacterial coinfection. The prevalence of bacterial coinfection and antibiotic use was 5.62% and 61%, respectively, most prevalent in North American studies (7.89%).
Most patients were males averagely aged 61 years. Cephalosporins were the most commonly used (88%) antibiotics, 39% of which were initiated on admission. The most commonly reported bacterial organism was S. aureus (40%), and the most common source of bacterial coinfection was the respiratory (50%).
Retrospective cohort studies had the highest bacterial coinfection prevalence (5.92%), whereas prospective cohort studies (77.83%) had the highest prevalence of antibiotic use. Antibiotic usage was reported in 73% of patients across 18/22 of included studies. North America had the highest antibiotic use in SARS-CoV-2 infections. (68.84%).
Conclusion
The study highlighted the need to improve the rationality of antibiotic prescription, indicated by the high prevalence of antibiotic prescription despite the low prevalence of bacterial coinfections. More targeted therapies need to be designed to decrease international AMR concerns.
Future studies with proportional global geographical representation and updated information based on studies conducted throughout the COVID-19 pandemic are required. These studies should consider the impact of new variants and treatment regimens, including the justification for antibiotic use, to increase the generalizability of the current study findings.
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Prevalence of Bacterial Coinfection and Patterns of Antibiotics Prescribing in Patients with COVID-19: A Systematic review and Meta-Analysis, Faisal Salman Alshaikh, Oula Nawaf Sindi, Brian Godman, R Andrew Seaton, Amanj Kurdi, medRxiv, 2022.03.02.22271779; doi: https://doi.org/10.1101/2022.03.02.22271779, https://www.medrxiv.org/content/10.1101/2022.03.02.22271779v1
Posted in: Medical Research News | Disease/Infection News
Tags: Antibiotic, Antimicrobial Resistance, Coronavirus, Coronavirus Disease COVID-19, Hospital, Influenza, Mortality, Pandemic, Pneumonia, Polymerase, Polymerase Chain Reaction, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Staphylococcus aureus, Syndrome, Transcription

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article