A remote military medical team can offer insights to US hospitals preparing for COVID-19

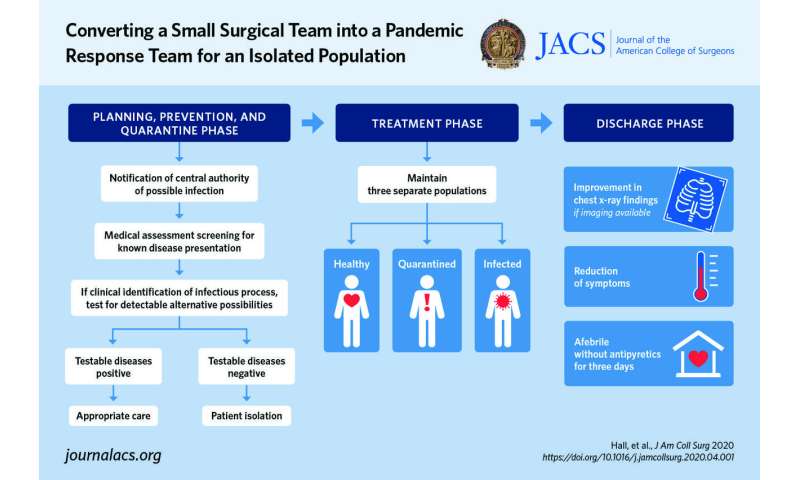
As the number of people infected with Coronavirus Disease 2019 (COVID-19) rises in the U.S. and around the world, hospitals are faced with difficult decisions for how to best provide care for a growing number of patients. The lessons learned by a small military surgical team who had to transition into a pandemic response team during the COVID-19 pandemic can offer insights for medical centers around the U.S. that are adapting in a rapidly changing environment. The medical team’s recommendations are published as the “article in press” on the website of the Journal of the American College of Surgeons ahead of print.
The surgical team is based in a remote region of Africa. They provide care for the active duty military population stationed there, which the authors describe as young and healthy, but supported by civilian personnel of various ages.
“The team members were trained and equipped for damage control resuscitation and surgery. No one had hands on experience with pandemics at home, so rifling through information for truths to familiarize ourselves was time consuming,” said lead author MAJ Andrew Hall, MD, FACS, Special Operations Command Africa, speaking for the team. “We cannot do many proposed cutting-edge therapies but have to rely on tried medical principles. We have many supply chain challenges that need to be factored in when planning a response.”
Military medical teams are typically focused on treating traumatic injuries and performing damage control surgery. As the threat of the COVID-19 pandemic grew, the team—consisting of a surgeon, an emergency medicine physician, a certified nurse anesthetist, an intensive care nurse, a scrub technician, and a medical planner—transitioned into an infectious disease containment and treatment team.
“This transition to a new primary medical mission in the face of a pandemic is applicable to any small medical team tasked with taking care of isolated populations,” the authors write.
The COVID-19 pandemic has created a situation where even in places where health care resources are typically abundant, hospitals are being forced to come up with creative solutions to provide care for the increasing number of critically ill patients with COVID-19 requiring medical treatment. Medical teams providing care around the world in regions that do not have abundant resources are used to adapting in innovative ways.
“It is essential to evaluate everyone’s skillsets and experience. It is not just the doctors. Everyone can have valuable skills to rely on,” Dr. Hall said.
Dr. Hall’s team was working with an isolated population, which presents its own unique set of challenges. During times of crisis, he said it’s important to learn to rely on non-medical labor to provide medical interventions. Specifically, he said things like refilling oxygen tanks can be done by non-medical providers. The tanks can be moved out of contaminated areas to be picked up and refilled, then brought back by non-medical personnel. He also said checks to ensure adequate lighting, temperature controls, and electrical outlets in the tents should be done. “Consider alternate sources for materials. For example, our metal fabricators made ICU beds out of spare materials,” he said.
However, he did say, “Thankfully, odds are in a small population’s favor in that not many people are going to get deathly ill. You must limit the spread, so those relatively rare events don’t statistically become likely. There are definite limitations to our capabilities, and we had to come to grips with those limitations and try to mitigate them as best as possible.”
Source: Read Full Article